GRAND FALLS-WINDSOR, N.L. — While Central Health wasn’t able to break down case figures, the regional health authority states it annually handles several thousand requests surrounding psychiatry – which can range from mental health promotion to psychiatric services.
To have services available to clients, Central Health has adopted a stepped-care approach that starts with a primary care provider or self-referral that builds towards psychiatrics appointments.
By using online services, and the introduction of walk-in counselling service – such as DoorWays – Diane Minhas, director of Mental Health and Addictions with Central Health, said wait times have been reduced from several weeks to one day.
“We have had a minimal or no wait list for the past four years,” she said.
However, this doesn’t apply to wait times for psychiatry.
Central Health doesn’t have firm numbers on this field. Minhas said a triage nurse will be working at establishing those waitlist times. This would be from the time of referral to an actual appointment.
The Central Regional Health Centre in Grand Falls-Windsor has six psychiatrists in place. A psychiatrist in Gander is closing their practice. Minhas said active recruiting for psychiatrists in Gander is taking place.
Minhas doesn’t foresee the loss of a phychiatrist causing delays in access to service.
She said service is prioritized and those in greatest need would still be seen within a timely manner.
“It’s not going to slow it down as much as it’s (about) having the right person in the right door at the right time,” she said.
Mental wellness
Which is why Roger Bull, chair of the Eastport Peninsula Recreation and Wellness Committee, is calling for a strong mental health approach in rural communities.
Bull said there are two main concerns, a lack of front line services and information distribution about said services needs to be addressed on the Eastport Peninsula.
“We don’t really know where to go, because there is nowhere to go here, it’s Gander or Grand Falls-Windsor,” he said.
The group started in January 2018, focusing on physical activity and healthy eating, but earlier this month made a shift towards mental wellness.
Bull said a buildup to mental wellness was a mandate from the start for the committee.
“And a few people from the community came forward and suggested we try and get something in place sooner rather than later,” he said. “It got us moving quicker than we normally would have.”
The committee held a public session Feb. 7, attended by approximately 60 people. The goal was to share information about mental health services available and to hear area concerns.
“We are trying to get things to a point where we are in a prevention mode,” he said. “This would be in the form of stress reduction techniques and building a community network of support.
“We want to establish something so when people are having a tough time, they have a place to come and share issues, so it doesn’t build up to the point where you have to go to Gander or Grand Falls for services.”
The meeting was held in conjunction with Central Health and the Canadian Mental Health Association. Bull said a steering committee will be formed to explore best approaches in offering programming.
“Living in a rural area you don’t expect to have the same level of service as a larger center, but still it could be better,” he said. “I’m hoping within a couple of months we will have a sense of what training programs we want to do.”
The initiative is being applauded by Dan Goodyear, CEO for the Canadian Mental Health Association, Newfoundland and Labrador.
“To me, having communities taking ownership is an essential ingredient in providing successful mental health programming,” he said.
And he feels the grassroots approach is a step in the right direction.
“We’re not going to get a physiatrist in every single town, but what we do need is access to the right service at the right time,” he said. “People need to know what type of services are in their community, and what kind of preventative things are in place.”
In central Newfoundland, the Canadian Mental Health Association has an office in Grand Falls-Windsor.
Goodyear said work is ongoing within schools through Talk Today, which provides suicide prevention training for adults attached to teams within schools, and Safe Talk, for young adults 15 and above.
The organization also does Healthy Relationships Plus, for children 12 to 18, to support mental wellness.
By having such services in place, he said, it provides quick access to those who need help.
And when a greater need for assistance arises, guidance towards professional help can be identified.
Central approach
Minhas sees the challenges in rural Newfoundland as well, and it’s something she said Central Health is trying to address.
“There is work taking place around clinic travel. In Botwood for example, once every week there is a metal health clinic held,” she said. “There are many services available through Telehealth, while maybe there’s not an actual person on the ground, there is still access to service.”
And she says the approach is about providing access to services to those who need it most.
“We are all citizens of Newfoundland and Labrador, and people throughout the province should have the same access, at least similar services, no matter where they are and that’s what we are trying to get to,” she said.
There is a need for mental health services in central Newfoundland, but that isn’t a bad thing, stated Minhas.
In the past mental health was stigmatized but it is now getting to the point where people are becoming comfortable in reaching out for help.
“Many years ago, people would hide away and they wouldn’t want anybody to know,” she said. “Nowadays, people accept mental health problems as a genuine problem.”
Mental health in Canada
- One in five Canadians will experience a mental health problem or illness.
- Approximately eight per cent of adults will experience major depression.
- The mortality rate due to suicide among men is four times the rate among women.
- It is estimated that 10-20 per cent of Canadian youth are affected by a mental illness or disorder.
- Almost one half (49 per cent) of those who feel they have suffered from depression or anxiety have never gone to see a doctor about this problem.
- Schizophrenia affects one per cent of the Canadian population.
- Anxiety disorders affect five per cent of the household population.
SOURCE: Canadian Mental Health Association
Accessing service in central
For those who need the assistance of mental health services within the central Newfoundland region, Diane Minhas, director of Mental Health and Addictions with Central Health, outlined a few key outreach points.
Walk in clinics
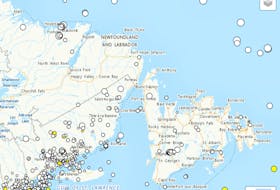
- James Paton Memorial Regional Health Centre, Gander – DoorWays – Tuesday, 1-4:30 p.m., Thursday, 8:30 a.m.-4:30 p.m.
- Central Regional Health Centre, Grand Falls-Windsor – DoorWays – Tuesday and Wednesday, 1-4:30 p.m., Thursday, 8:30 a.m.-4:30 p.m.
- Lewisporte Community Health Centre – DoorWays – Thursday, 1-4:30 pm
- Green Bay Health Centre, Springdale – DoorWays – Wednesday, 1-4:30 p.m.
- St. Alban’s Community Health Centre – DoorWays – Wednesday, 1-4:30 p.m.
- Dr. Hugh Toomey Health Centre, Botwood – Mental Wellness Clinic – 9 a.m.-4 p.m.
Anyone in a mental health crisis can also go to the nearest emergency department.
Phone numbers
- Central Health Mental Health and Addictions Services toll-free triage line – 1-844-353-3330.
- Mental Health Crisis line 1-888-737-4668
- 911